|
As a result of the continued consequences of the Coronavirus Disease 2019 (COVID-19) pandemic, on this date and after consultation with public health officials as necessary, I, Xavier Becerra, Secretary of Health and Human Services, pursuant to the authority vested in me under section 319 of the Public Health Service Act, do hereby renew, effective January 11, 2023, the January 31, 2020, determination by former Secretary Alex M. Azar II, that he previously renewed on April 21, 2020, July 23, 2020, October 2, 2020, and January 7, 2021, and that I renewed on April 15, 2021, July 19, 2021, October 15, 2021, January 14, 2022, April 12, 2022, July 15, 2022, and October 13, 2022, that a public health emergency exists and has existed since January 27, 2020, nationwide.
0 Comments
New contracts will advance health equity, quality, access, accountability, and transparency to improve the Medi-Cal health care delivery system.
“We are committed to setting the stage for Medicaid transformation across the country as well as for broader health system innovation within California.” The State’s top priority is to ensure that Medi-Cal members have access to health insurance plans that provide high-quality and timely care and are focused on delivering on the State’s transformations that are designed to move the health system to become person-centered, equity-focused, and data-driven. Click here to read the entire press release. Here is a notice from the Medical Board of California - It is about a sign to hang in waiting rooms and later on-line on websites!
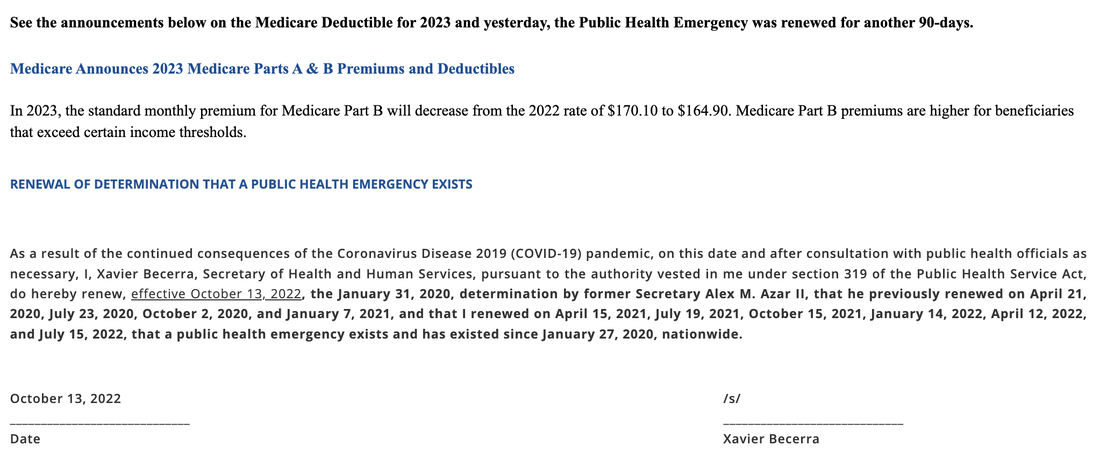
"The federal Physician Payments Sunshine Act requires that detailed information about payment and other payments of value worth over ten dollars ($10) from manufacturers of drugs, medical devices, and biologics to physicians and teaching hospitals be made available to the public." It has a section about not applicable to emergency room physicians but does not address inpatient providers? - 665. This article does not apply to a physician and surgeon working in a hospital emergency room. The searches are available for 2021 payments received and are very interesting. Here is the link. The U.S. will extend the COVID-19 public health emergency past January 11, 2023, CNBC reported Nov. 11. A 12th extension of the PHE since the first in January 2020 is also likely because of a lack of public statement from HHS warning about a termination. The agency last renewed the PHE Oct. 13 for an additional 90 days to Jan. 11, 2023 — it also told states it would provide a notice 60 days before if it did decide to end it, or Nov. 11.
The PHE allows the country to continue operating under pandemic-era policies, which led to a complete overhaul of telehealth and who can use it, fast-tracked approvals of COVID-19 vaccines and treatments, and preserved healthcare coverage for millions of Medicaid beneficiaries nationwide. Eleven states also still have coinciding public health emergency orders in place. As of now, Medicare telehealth flexibilities will end 151 days after the PHE expires. In July, the House passed The Advancing Telehealth Beyond COVID-19 Act, but the legislation must still be approved by the Senate for Medicare patients to continue using telehealth through 2024. "It's not that we necessarily want to continue the PHE for a long period of time," Nancy Foster, AHA's vice president of quality and patient safety, told Becker's in October. "What has not yet happened is fully thinking through how to unwind some of the [telehealth] flexibilities we currently have, and how to perhaps make permanent some of the others." In addition, the end of the PHE will trigger a Medicaid redetermination process that will cause a major disenrollment of beneficiaries. Over the course of about a year, HHS estimates up to 15 million people could lose health coverage. Payers are prepping for the redetermination period, as they expect to lose Medicaid members and hope to switch some to ACA coverage. With the Inflation Reduction Act's extension of ACA premium tax credits through the end of 2025, the nation's largest insurers have all recently announced plans to majorly expand exchange offerings in 2023, including UnitedHealthcare, Elevance, Aetna, Cigna and Centene. The extension of the federal emergency past January may have been unexpected for insurers, as UnitedHealth Group executives told investors Oct. 14 they thought the PHE would end in January. "Our tailwinds will be weighed against one known headwind, and that is the membership attrition and related impacts on our Medicaid business as eligibility redeterminations are conducted over the course of the next year," Elevance Health's CFO John Gallina told investors Oct. 19. The extension also comes amid uncertainty around public health as winter looms. New Omicron strains — dubbed "escape variants" for their immune evasiveness — have become the dominant strains in the U.S., accounting for 40 percent of all cases in the week ending Nov. 12. Daily cases in the country are expected to grow 39 percent from Nov. 3-17. Hospital admissions trends are expected to remain stable or be more uncertain, with 1,300 to 7,300 new admissions likely reported on Nov. 25, according to the CDC. As of Nov. 4, the nation's seven-day average of new hospital admissions was 3,273. Advanced has had a written compliance manual for many years now. It was created from the regulations set up by the OIG for Third Party Medical Billing Companies (us) to make sure that we are following the guidelines set in place. Our clients receive a copy of our manual at the beginning of our services so the roles are clear and everyone knows what is expected of them.
Some of the highlights are :
Compliance is not exciting or fun but needed in the healthcare industry to follow the rules that have been set up to follow. It's like the Monopoly game, you can win if you read the rules on the back of the box. By now you have probably heard about the No Surprise Medical act that was passed in December 2020 and takes effect January 1, 2022. It is intended to protect patients from receiving bills from Out of Network providers while seen at in-network facilities. It would limit the patients out of pocket charge to the in network median rate.
The health plan has 30-days from receiving the claim to negotiate a payment rate. The provider then has 4 days from the time of receiving the payment to file an independent dispute resolution process to determine a different payment amount. This will then go to arbitration and the arbiter will look at several different factors - the providers expertise, the median in-network rate and complexity of the service provided. There are separate rules if the patients health plan is a Federal plan, is in a different state than the provider is or if they have paid the payment to the patients already? It is very confusing. The exact policies are still being defined:
We met an attorney at the HBMA conference in September and he specializes in fighting the insurance companies for the low payments that are sometimes made. We will keep you posted if we see any out-of-network payments made for patients seen at in-network facilities. CMS released its annual proposed changes to the Physician Fee Schedule for 2022, which expands certain Medicare telehealth provisions and updates the payment rate for physician services.
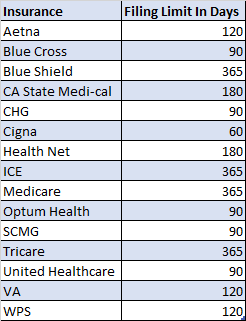
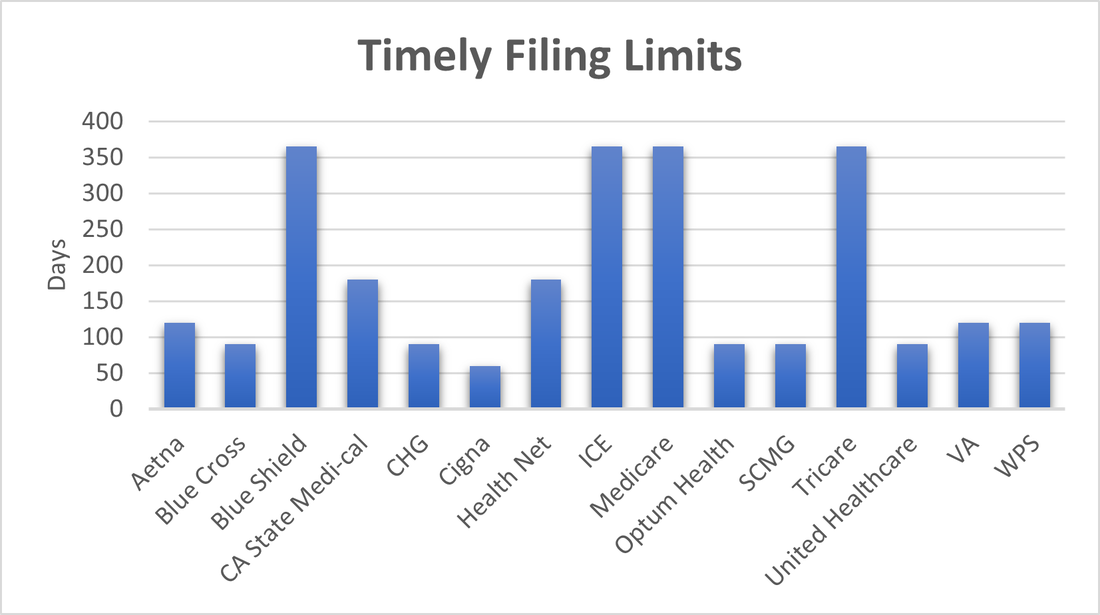
Each year there are updates to the Physician Fee Schedule and the “Proposed Rules” enter into a comment period where providers and healthcare industry organizations weigh in on those proposed changes. This year they are as important as ever. We are all familiar with insurance timely filing limits. Those deadlines listed in your provider contracts and manuals that state the amount of time after the date of service that you have to submit your claims to the insurance. Anything received after this time frame will automatically be denied for past timely filing limits and you will not be paid for these services. We wanted to review some of the most common filing limits that we have recently seen within our providers contracts and in published insurance manuals. These show the importance of turning in your billing timely and asking patients at each visit if their insurance has recently changed.
“While 62% of breaches in 2020 were related to hacking, healthcare insiders themselves accounted for 1 in every 5 breaches.”
We hear about healthcare breaches almost every day lately. Insurance companies that had a breech and had millions of records accessed, healthcare systems that were subject to hackers and even providers themselves losing track of PHI. Even if you do not host your patient health information directly, you need to always be aware and continue to monitor the systems you have in place, to make sure the information is being guarded at all times. Who is in charge of your internal passwords, setting up new users, terminating employees that have left? When did you last do a Security Risk Assessment? These are questions that you should be reviewing at least quarterly and documenting the outcomes. |
Categories
All
Archives
January 2023
|
|
© COPYRIGHT 2021. ALL RIGHTS RESERVED.
Privacy Policy Terms of Service |